Abstract

Introduction: Graft failure (GF) is an infrequent but serious complication of following matched related or unrelated donor peripheral blood stem cell transplantation. Although infusion of CD34+-selected stem cells without additional conditioning is currently one strategy to treat this complication, few studies have reported predictors of response.
Methods: We report the outcome of consecutive patients identified at two UK transplant centres between 1999 and 2017 who had primary or secondary GF after an allogeneic peripheral blood stem cell transplant and who underwent a CD34+ selected stem cell infusion without further conditioning. GF was confirmed by chimerism, bone marrow examination and exclusion of relapsed disease. Primary GF was defined by failure to ever achieve count recovery in one or more lineages (neutrophils >0.5x109/L, untransfused platelets >20 x109/L and untransfused Hb >8 g/L) post transplantation. Secondary GF was defined by loss of counts after the initial achievement of engraftment. A complete response (CR) was defined as haematological improvement (HI) in all cell lines (Hb>8g/L, platelets > 30x109/L and neutrophils > 1.5x109/L). A partial response (PR) was defined as HI within the first 30 days but not in all cell lineages. Responses were categorized as early (<30 days after infusion) versus late (>30 days); in the latter case, the role of the CD34+ infusion in count recovery was not known.
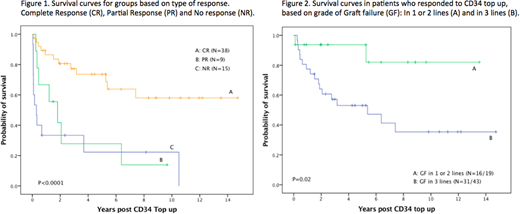
Results: We identified 62 patients with GF, male:female 35:27, with a median age of 43 years (range, 10-66). Fifty-six patients (90%) had had reduced intensity conditioning. Median follow up was 6.4 years. Diagnoses included acute leukemia (n=18), non-Hodgkin's lymphoma (n=18), Hodgkin's Lymphoma (n=7), MDS (n= 6), multiple myeloma (n=3), myelofibrosis (n=2), CLL (n=2), severe aplastic anaemia (n=2), primary immunodeficiency (n=2), CML (n=1) and sickle cell disease (n=1). The original graft source was peripheral blood stem cells from a matched related donor (n=29), matched unrelated donor (n=18) and mismatched unrelated donor (n=15). Twenty-one (34%) patients had primary GF and 41 (66%) had secondary GF. Forty-three patients (69%) had GF in all 3 lineages and 19 patients (31%) had GF in 1 or 2 lineages. The median CD34+ cell dose/kg recipient weight was 3.2 x 106/kg (range, 0.47-14.2 x 106/kg) at a median of 181 days (range, 21-2718 days) following transplant. No response to CD34+ infusion was seen in 15 (24%) patients. Of the remaining 47 patients who responded (76%), 19 patients achieved a CR <30 days, 19 patients had a CR >30 days, 5 had a PR <30 days and 4 had a PR >30 days. Of those who responded, the median number of days required for neutrophil recovery was 29 days (6-1182), platelets recovery was 18 days (5-600) and haemoglobin recovery was 25 days (6-511). In a multivariate analysis, parameters significantly associated with response were CMV serostatus negative for both patient and donor (OR: 20.12, CI 95%= 1.6 - 248) and matched patient/donor sex (OR: 73, CI 95%= 3.3- 1605). Other factors including CD34+ dose, unrelated/related donor, underlying disease, disease risk score, timing of infusion, recipient/donor age, primary or secondary GF and presence or absence of GVHD did not predict for response. Overall survival (OS) for all patients at 1 and 5 years was 70% (95% CI 58-82) and 54% (95% CI 41-68) respectively. OS at 1 and 5 years was 86.4% (95% CI 75-98) and 73.6% (95% CI 54-92) in patients showing a CR versus 66.7% (95% CI 35-98) and 27.8% (95% CI 3-60) in patients with PR (Figure 1). Patients showing no response had poor outcomes with OS of 33.3% (95% CI 9-58) and 22.2% (CI 95% 5-47) at 1 and 5 years. In responding patients, those who initially had GF in 1-2 lineages had 5-year OS of 93.8% (95% CI 82-99) versus GF in 3 lineages who had a 5-year OS of 53% (95% CI 34-88) (Figure 2).
Conclusions: This analysis represents the largest report of outcomes in patients who have received a CD34+ selected stem cell infusion without conditioning for GF. Negative donor/recipient CMV serostatus and sex matching predicted response. In responding patients, GF initially affecting <3 lineages was a predictor of better OS at 5 years. New strategies including cytokine or agonist support, or second transplant need to be investigated in partially or non-responding patients.
Hough:University College London Hospital's NHS Foundation Trust: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal